Standards of Practice
Association of Hearing Instrument Practitioners of Ontario
Standards of Practice
Overview
To ensure high standards of equipment and techniques in the testing of hearing, selection and fitting of hearing instruments and associated devices, and where the practice includes it, in the removal of cerumen from the external ear canal as per section 9.1.3 of the Association By-Laws.
1.0 Purpose of Policy
1.1 Maintenance of high standards by all members is in the best interest of the hard of hearing and the profession.
1.2 These standards are the minimally acceptable level of standards with respect to equipment, testing of hearing, selection and fitting of hearing instruments and associated devices.
2.0 Scope of Practice
2.1 Members must practice within the limit of their competence as determined by their education, training and professional experience.
2.2 The Scope of Practice of the Hearing Instrument Specialist H.I.S. and Hearing Instrument Dispenser H.I.D. is outlined within the Association By-Laws, Articles 3.1.1 and 3.1.2.
2.3 Members must make appropriate referrals to other healthcare individuals when encountering procedures that exceed their limits of competence or scope of practice.
2.4 “Must” statements establish standards that members must always follow.
2.5 Members may exercise professional judgement, taking into account the environment(s) and their patients’/clients’ needs when considering deviating from the guidelines. The reason(s) why guidelines were not followed must be recorded.
2.6 A “Contraindication” is a specific situation in which a procedure cannot be performed because it may have a negative effect or cause harm to the patient/client.
3.0 Restrictive Activities (Prescription)
3.1 Members will not violate any law, rule or regulation applicable to the provision of hearing instruments and associated devices.
3.2 As per section #31 (Dispensing Hearing Aids) of the Regulated Health Professions Act 1991 S.O. 1991, c. 18. “No person shall dispense a hearing aid for a hearing impaired person except under a prescription by a member authorized by a health profession Act to prescribe a hearing aid for a hearing impaired person.” Prescription of a hearing aid is an authorized act under the Medicine Act, 1991 S.O. 1991, c.30 and the Audiology and Speech-Language Pathology Act, 1991, S.O. 1991, c.19.
4.0 Referral to Physician
4.1 The patient/client must be referred to a physician for medical clearance as per Ontario Medical Association – Red Flag List (See Appendix A).
5.0 Insurance
5.1 Members must ensure they carry Professional Liability Insurance for a minimum of $2,000,000.
5.2 A copy of Certificate of Insurance must be submitted to the AHIP office with the completed membership renewal application by the 31st of December of each year.
6.0 Equipment Requirements
6.1 Hearing Instrument Dispenser H.I.D. required equipment:
- High resolution otoscope
- Programming interface.
- Electro-acoustic hearing instrument analyzer
6.2 Hearing Instrument Specialist H.I.S. required equipment:
- High resolution otoscope
- Programming interface.
- Electro-acoustic hearing instrument analyzer
- Sound attenuation booth
- A diagnostic audiometer with air conduction, bone conduction, narrow band masking noise, speech audiometry and speech masking noise capabilities that utilize insert and/or TDH style transducers.
- Full range acoustic immittance measurement system for tympanometry and acoustic reflex measures
- Real ear measurement system
6.3 All equipment that is not self-calibrating must be calibrated annually in accordance with current ANSI standards. Equipment must be in proper working order at all times.
6.4 A copy of current calibration certificate must be submitted to the AHIP office upon request.
7.0 Testing Environment
7.1 The testing environment must meet one of the following requirements:
- Within a sound attenuation booth
- Outside a sound attenuation booth
7.2 When testing outside a sound attenuation booth, every effort must be made to ensure the ambient noise level in the room does not exceed 40dB SPL. Use of a sound level meter is recommended to determine the noise level in the room. The acoustic characteristics of the room must be recorded on the audiogram form.
8.0 Assessment Protocol
8.1 A complete hearing assessment must include the following components (See Appendix B), unless contraindicated.
- Case History
- Otoscopy
- Impedance Audiometry (Acoustic Immittance):
- Tympanometry
- Acoustic Reflex
- Pure Tone Audiometry:
- Air Conduction Testing (AC)
- Bone Conduction Testing (BC) as necessary
- Speech Audiometry:
- Most Comfortable Level (MCL)
- Speech Reception Threshold (SRT)
- Speech Awareness Threshold (SAT)
Test will be performed when SRT may not be obtained - Word Recognition Scores (WRS)
- Speech-In-Noise (SIN) as necessary
- Loudness Discomfort Level (LDL)
- Masking as necessary
- Tinnitus:
- Assessment
- Counselling
- Follow up care
9.0 Recording Test Results
9.1 The results of each hearing assessment must be recorded on the audiogram form.
9.2 Symbols used to record air conduction, bone conduction and masking thresholds must be noted in a key on the audiogram form.
9.3 All audiogram symbols must conform to current ASHA standards (American Speech-Language-Hearing Association 1990)1.
10.0 Selection and Fitting of Hearing Instruments and Assistive Listening Devices
10.1 Selection and fitting of hearing instrument(s) must be in accordance with the following, unless contraindicated.
- Complete hearing assessment
- A new hearing assessment must be completed if more than six (6) months has elapsed since the last hearing assessment
- In situations where it is not possible to have a new hearing assessment completed, the reasons must be recorded.
- Ear Impression as necessary
- Programming of the hearing instrument(s)
- Instruction and counseling for the proper use and care of the hearing instrument(s) and/or assistive listening device(s)
- Verification of the benefit of the hearing instrument(s)
- In all cases where a patient/client is fitted with the hearing instrument(s), the Member must allow the patient/client a minimum thirty (30) day trial period
- Maintain an ongoing follow-up service to encourage the continued use of the hearing instrument(s) and/or assistive listening device(s)
- Repairs and maintenance of the hearing instrument(s), assistive listening device(s) and accessories
1http://www.asha.org/policy/GL1990-00006/
11.0 Ear Impression
11.1 Ear impressions are taken to fabricate products for amplification and hearing/ear protection.
11.2 Hearing Instrument Specialist H.I.S. and Hearing Instrument Dispenser H.I.D. are ethically responsible to ensure they are competent in ear impression taking and to keep their patient/client safe during the procedure.
11.3 The ear canal must be examined with an otoscope prior to taking an ear impression and after the removal of the ear impression.
11.4 Infection control must be followed to ensure the health and safety of the patient/client and Member. Infection control procedures include but are not limited to: hand washing, waste management and criteria for disinfection and sterilization. Refer to 5.01 Ear impression procedures in Infection Control Policy.
11.5 Equipment requirements:
- Otoscope with speculum
- Earlight with removable tip
- Otoblock with thread
- Syringe or impression gun
- Impression material
11.6 Contraindications, subject to medical clearance:
- Impacted or excessive cerumen in the ear canal
- A foreign body in the ear canal
- External and/or middle ear condition
12.0 Fitting Verification
12.1 Verification procedures are an essential component of successful hearing instrument fittings.
12.2 Hearing aid recommendations must be verified to ensure appropriate amplification, unless contraindicated.
12.3 Real Ear Measurements (REMs), also known as probe microphone measures, are the preferred method, specifically in situ REM using probe tubes rather than coupler measures.
12.4 Real Ear Measurement measures the performance of a hearing instrument in the patient’s/client’s ear to ensure sounds are audible, comfortable and tolerable across the frequencies of the patient’s/client’s reduced dynamic range.
12.5 The results must be recorded including patient’s/client’s name, date and hearing aid serial number(s).
13.0 Records
13.1 Records of all tests performed and/or subsequent follow-up services must be recorded.
13.2 All records relating to the services provided to the patient/client including the case history, audiogram, all results of testing including verification, referral information and follow-up services and dates will be kept on file for a minimum period of seven (7) years or ten (10) years past the 18th birthday of a minor.
14.0 Clinical Placements and Internship
14.1 Students completing clinical placement or graduates completing the Hearing Instrument Specialist H.I.S. Internship Program will only complete those tasks that are geared to their level of competence under the supervision of a Hearing Instrument Practitioner, Member in good standing of AHIP or an Audiologist, in good standing registered under CASLPO.
14.2 All students on clinical placement must be covered under the respective educational institution Professional Liability Insurance.
14.3 All Interns must have Professional Liability Insurance coverage.
15.0 Continuing Competencies
15.1 In order to maintain membership in the Association, a minimum of twelve (12) hours of AHIP approved, Continuing Education Units (CEU’s) must be obtained per calendar year as outlined within the Association By-Laws, Article 9.1.2 (ii).
References
Audiometric Symbols. (1990). Retrieved March 9, 2015, from http://www.asha.org/policy/GL1990-00006/
Appendix A
Referral to Physician
The patient/client must be referred to a physician for medical clearance in each of the following instances (Ontario Medical Association – Red Flag List):
- Asymmetric sensorineural hearing loss (>10 dB PTA and/or discrimination score difference>12%)
- History of injury to ear or head
- History of weakness of the face
- Prior history of ear surgery, excluding myringotomy
- History of drainage from the ear within the previous 90 days
- History of dizziness or vertigo
- Pain or discomfort in the ear within the previous 30 days
- A significant change in hearing within the previous 90 days (>10 dB or 12 % change in discrimination score)
- Audiometric air-bone gap equal to or greater than 15 decibels at 500 Hz, 1000 Hz and 2000 Hz
- Age of 18 years or younger
- Visible deformity of the ear (including perforation of the tympanic membrane)
- Unilateral tinnitus
- History of hearing loss in the family (other than age-related)
- History of exposure to ototoxic drugs
- History of meningitis
- Suspicion of exaggerated hearing loss
- History of exposure to loud noise
- Excessive cerumen (wax) or a foreign body in the ear canal
- Any person that the hearing health care professional feels should be seen by a physician
Appendix B
- Case History
A case history will contain but not be limited to the following patient/client information:
a. Name, address and phone number
b. Date of Birth
c. OHIP number
d. VAC or WSIB insurance number
e. Third party insurance number when billed directly by the Member
f. History of hearing loss, onset, duration
g. Medical history infections, allergies, surgeries, medications
h. Family history of hearing loss
i. History of noise exposure
j. History of tinnitus, pain, dizziness, vertigo
k. History of hearing aid use
l. Expectations and needs of the patient/client, lifestyle
m. Date of last history take
- Otoscopy
An otoscopic exam must be completed prior to any hearing assessment, impedance audiometry, real ear measurement and before and after impression taking. The purpose of the otoscopic exam is to:
a. Evaluate the possibility of ear canal collapse
b. Observe any external and/or middle ear condition
c. Determine the presence of cerumen
d. Determine the size of the external canal and its ability to accommodate a dome, earmold or hearing instrument
e. Determine the location of the second bend of the ear canal and other landmarks when taking an ear impression
- Impedance Audiometry (Acoustic Immittance)
a) Tympanometry
Tympanometry is a measurement that gives information regarding the condition of the tympanic membrane and middle ear space.
b) Acoustic Reflexes
The acoustic reflex threshold is the lowest intensity needed to elicit a contraction of the stapedius and tensor tympani muscles using a pure tone stimulus. Acoustic reflex measures can be conducted either through an ipsilateral or contralateral presentation. Contralateral reflexes are measured by stimulating one ear and measuring the reflexes of the opposite ear.Ipsilateral reflexes are measured by stimulating and measuring the same ear.
- Pure Tone Audiometry
a) Air Conduction Testing (AC)
The purpose of air conduction testing is to specify the amount of hearing sensitivity at various frequencies. If there is a hearing loss, air conduction test results can specify the degree of hearing loss but not whether the deficit is produced by abnormality in the conductive mechanism, sensorineural mechanism, or both.
b) Bone Conduction Testing (BC)
The purpose of bone conduction testing is to determine sensorineural sensitivity. The prominent bone behind the ear (mastoid process) is the common place from which the bone conduction measurements are made. The range of frequencies to be tested and the maximum intensities emitted are more limited for bone conduction than for air conduction.
- Speech Audiometry
a) Most Comfortable Level (MCL)
Intensity level at which sound is perceived to be most comfortable
Measurement of MCL is obtained using a continuous-discourse stimulus to give the patient/client the opportunity to listen to speech as it fluctuates over time.
b) Speech Reception Threshold (SRT)
The lowest level at which speech can be understood 50% of the time. SRT is obtained using spondaic words. Words may be presented to the patient/client through monitored live voice or by the use of pre-recorded word list.
c) Speech Awareness Threshold (SAT)
The lowest level at which speech can barely be detected. SAT is obtained using spondaic words. Words may be presented to the patient/client through monitored live voice or by the use of pre-recorded word list.
d) Word Recognition Scores (WRS)
The test presentation level is at the patient’s/client’s MCL. WRS is obtained using single-syllable words. Words may be presented by monitored live voice or pre-recorded word list.
e) Speech-in-Noise (SIN)
Speech-in-noise testing measures the ability to hear in noise. Speech understanding in noise cannot be reliably predicted from the pure tone audiogram or other standard audiometric tests. SIN testing results will help in the selection of the most appropriate amplification strategy and counselling about realistic expectations.
f) Loudness Discomfort Level (LDL)
The hearing level at which a patient/client finds speech uncomfortably, but not painfully, loud. LDL provides an estimate for the dynamic range for speech which is the difference between SRT and LDL.
- Masking
Masking is the act of applying a signal (usually noise) to the non-test ear, to keep it from responding for the ear being tested.
Both unmasked and masked thresholds are shown on the audiogram.
There is no one universally correct procedure for masking. The most common masking procedure is the plateau method.
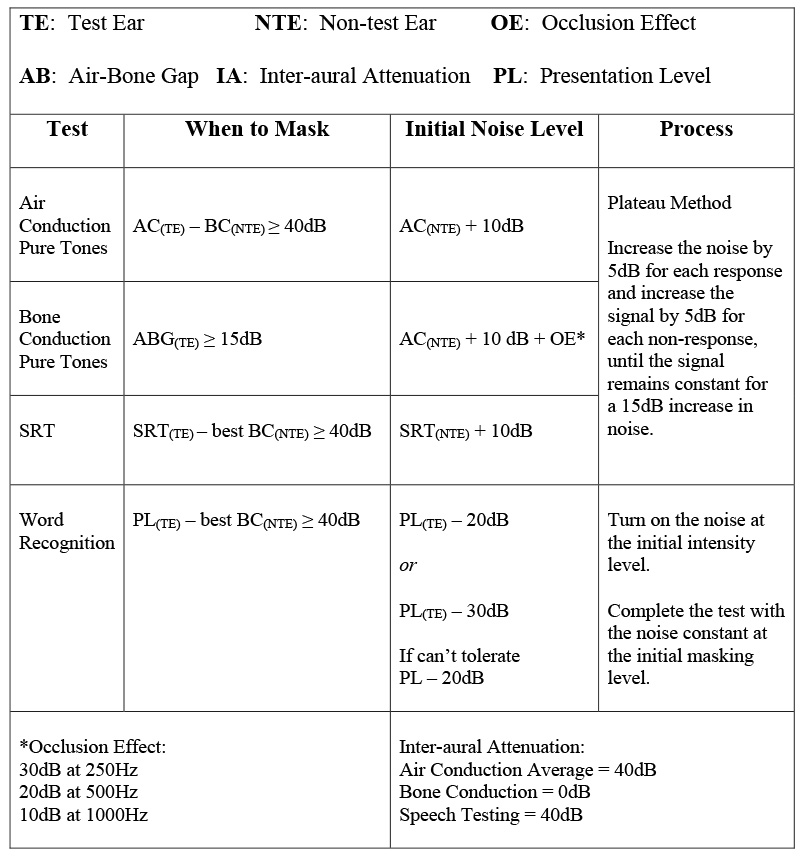
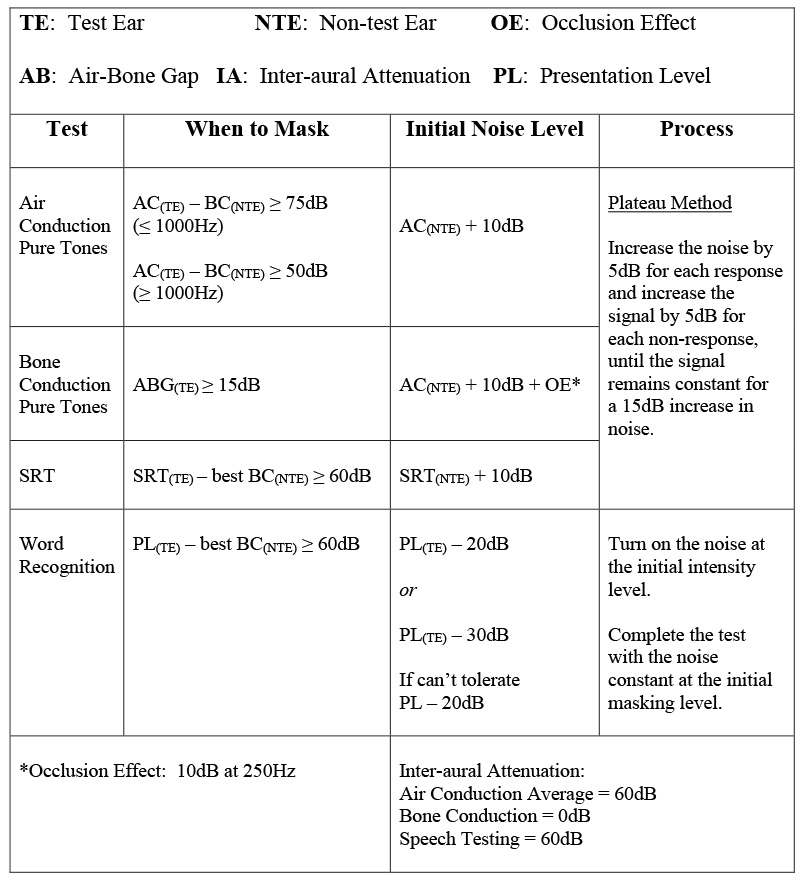
See charts #1 and #2 which summarize masking protocols, based on the plateau method of masking for TDH39 and insert earphones.
Chart #1 and #2: masking values and protocols were provided to AHIP by the Hearing Aid Practitioner program at MacEwan University in March 2015. The information is consistent with the MacEwan University curriculum taught in the winter 2015 term but is subject to change.
Masking Protocol: TDH39
Chart #1
Masking Protocol: Insert Earphones
Chart #2
References
Donaldson, L. (1999). Masking: Practical Applications of Masking Principles and Procedures (3rd ed.). Livonia, MI: International Hearing Society.
(1993). Distance Learning for Professionals in Hearing Health Sciences (5th ed.). Livonia, MI: International Hearing Society.
(2013). Trainer Manual. Livonia, MI: International Hearing Society.
Katz, H., Medwetsky, L., Burkard R., & Hood L. (2009). Handbook of Clinical Audiology (6th ed.). Baltimore, MD: Lippincott Williams & Wilkins.
Martin, F. N., & Clark, J. G. (2003). Introduction to Audiology (8th ed.). Boston, MA: Pearson Education, Inc..
