The eyes have it when it comes to identifying the ear complaints that most frequently present in primary care
By Rick Y. Fox, M. D., F.R.C.S. (C.) – Editor and Contributing Author – Dr. Fox has been a staff member at St. Joseph’s Health Centre in Toronto for 23 years, and is currently Chief of the division of Otolaryngology – Head and Neck Surgery. He is an Assistant Professor, Department of Otolaryngology, University of Toronto. Dr. Fox has a special interest in Otological Disorders.
Special thanks to Dr. Michael Hawke for supplying the images in this presentation. Dr. Hawke is a Professor Emeritus, Department of Otolaryngology-Head and Neck Surgery at the University of Toronto. He is known both Nationally and Internationally for his basic and clinical research in diseases of the ear and sinuses.
Some estimates suggest that upwards of 20 to 50% of patient visits to the family doctor’s office and the emergency department can be attributed to otolaryngic disorders. Many of these cases involve problems with the middle and external ear, such as otitis media, a particularly common condition experienced by 75% of the Canadian population by age one.
Small wonder, then, that undergraduate and graduate medical school training in these disorders is relatively limited. While some middle- and external-ear conditions are innocuous or symptomatically bothersome at worst, others are considered serious and may require surgical intervention. If left untreated (or undertreated), in some cases, patients can experience significant discomfort and even permanent hearing loss.
As with most illnesses, quick identification and treatment of these conditions are integral to achieving satisfactory outcomes.
In this, the otoscope and a familiarity with the visual clues for each presentation are the clinician’s best friends, as is a thorough grasp of established treatment protocols.
What follows is a visual tour of some of the hallmarks of middle- and external-ear disease most likely to appear in primary care.
Review Questions
Acute Otitis Externa
Otitis externa is typically a diffuse infection of the external canal skin involving Pseudomonas aeruginosa. It may also be caused by fungi such as Candida albicans or Aspergillus niger. Predisposing conditions are moisture or trauma. Symptoms include pain, hearing loss, and discharge, while treatment consists of topical preparations and debridement.
Chronic Otitis Externa
Recurrent acute infections may lead to chronic dermatitis of the external canal. Other contributing factors include eczema and psoriasis. Treatment may involve long-term use of topical agents with regular debridement.

Auricular Hematoma
Auricular hematoma is the result of blunt trauma or injury to the external ear, and arises when the subperichondrial space fills with blood. If left untreated, complications including infection and even permanent deformity (cauliflower ear) may result. Management consists of hematoma evacuation via repeat aspiration or, more commonly, by adequate incision and drainage with pressure dressing.

Perichondritis
Perichondritis and chondritis are infections of the perichondrium and cartilage of the ear most commonly caused by P. aeruginosa. Symptoms include pain, erythema and edema. Treatment may include topical, oral, or intravenous antibiotics.

Gout
(small superior lesions known as “tophi”)
Gouty tophi of the ear are superficial, well-circumscribed deposits in the oracle with no surrounding erythema or ulceration. Serum uric acid (sUA) will generally be elevated in these patients. Medication may be used to lower sUA levels in systemic gout, while the tophi may be removed for cosmetic reasons.

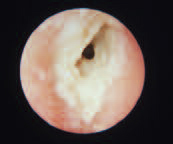
Exostoses
Exostoses are the most common asymptomatic growths found in the external auditory canal. They consist of dense, ivory-like compact bone. Repeated exposure to cold water is often the cause, and hence it is often referred to as “surfer’s ear.” Treatment is rarely required unless the extoses are particularly large and occlude the canal.
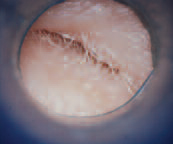
Deep Impacted Wax
Cerumen is a natural product of glands in the external canal. Impacted wax may result from the use of Q-tips, earplugs, or earphones. Hearing aids may also contribute to wax impaction. In some cases, cerumen softeners may be required before any removal is attempted.

Keratosis Obturans
Keratosis obturans of the external auditory canal is characterized by the accumulation of large plugs of squamous debris. It may present with both pain and hearing loss – erosion of the bony canal may also occur. Treatment consists of periodic removal of accumulated material.

Acquired Stenosis
(right external ear canal, from chronic Q-tip abuse)
Repeated minor trauma may result in scarring and subsequent stenosis, or narrowing, of the external auditory canal. Infections such as chronic otitis externa may result in a similar presentation.
Osteoma
(external ear canal)
Osteoma typically presents as a single, large pedunculated growth near the lateral end of the bony portion of the external auditory canal. If it is large enough, it may present with discomfort or hearing loss. If symptomatic, treatment involves surgical removal.
Infected Furuncle
(right ear)
A furuncle is a localized abscess surrounding a single hair follicle. These are usually caused by bacteria such as Staphylococcus aureus. Treatment consists of systemic and topical antibiotics, but incision and drainage may also be required.

Herpes Zoster
(note blisters)
Herpes zoster oticus (Ramsay Hunt syndrome) is a viral infection affecting the facial nerve. It is caused by the varicella virus, and is manifested by facial paralysis and herpetic vesicles in the external auditory canal and conchae. Severe pain is common. It is the second most common cause of facial paralysis after Bell’s palsy. Treatment options include systemic corticosteroids and antiviral agents.
Necrotizing Otitis Externa
Necrotizing otitis externa is a potentially life-threatening illness. It typically occurs in insulindependent diabetics, but any patient who is immunocompromised is also at risk. The main causative organism is P. aeruginosa. The disease is characterized by pain and discharge, and may progress to facial nerve paralysis or other cranial nerve palsies. Treatment consists of longterm systemic antibiotics and debridement.

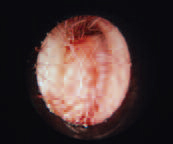
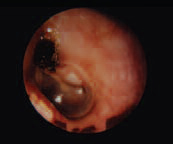
Bullous Myringitis
Bullous myringitis is characterized by serous or hemorrhagic blebs (small blisters) on the surface of the tympanic membrane. It may produce severe pain and hearing loss. The primary cause is thought to be viral or possibly due to Mycoplasma pneumonia infection. Treatment is symptomatic; the blebs can be opened in an attempt to relieve pain.

Granular Myringitis
(note reddish moist area)
Granular myringits may result from inadequate treatment of otitis externa. It is characterized by foul discharge and the appearance of granulation tissue on the surface of the tympanic membrane. Treatment consists of topical antibiotics and maintaining a dry ear.
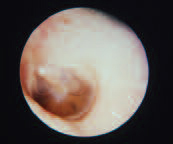
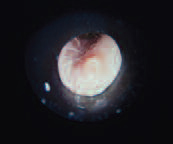
Serous Right Otitis Media with Effusion
Eustachian tube dysfunction may result in the accumulation of fluid in the middle ear space. Common causes are upper respiratory tract infections, allergies or barotrauma. Hearing loss is the main symptom. These are often self-limiting conditions, but treatment options include decongestants or myringotomy for chronic cases.

Early Acute Otitis Media
(right ear)
More common in the pediatric population, this condition may present with hearing loss and pain. In this photo, pus can be seen accumulating in this middle ear. In some cases, complications such as mastoiditis may occur. Antibiotics cam be prescribed for persistent pain or fever.

Mucoid Otits Media
When fluid remains in the middle ear for an extended period of time, it may develop into a thick, tenacious material. Thus, this condition is commonly referred to as “glue ear.” Hearing loss is the most common symptom and pain is usually not present.

Tympanosclerosis
Tympanosclerosis is the accumulation of hyaline material, or white plaque, in the fibrous layer of the tympanic membrane. It often occurs secondary to recurrent otitis media, or may develop post surgery. Treatment is not typically necessary.
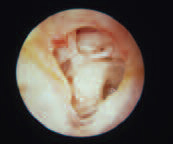
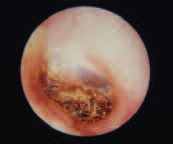
Perforation and Tympanosclerosis
(left ear)
In this photo, chronic infection has caused destruction of the tympanic membrane. Note the chronic scarring and ossicular damage. In these cases, it is imperative to keep the ear dry.
Retraction Pocket
(right ear)
If left untreated, chronic otitis media may result in retraction of the tympanic membrane. In this case, the central portion of the drum is seen to be retracting medially due to the negative pressure in the middle ear space. Ventilation tubes may reverse the process and restore normal middle ear function.

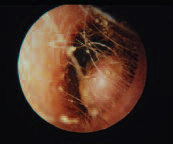
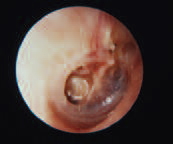
Retraction Pocket and Myringostapediopexy
In this photo, posterior retraction is severe and has resulted in ossicular destruction. The tympanic membrane adheres tightly to the stapes, and the incus has been eroded. Depending on symptoms and presence of hearing loss, treatment options include a range from simple observation to middle ear reconstructive surgery.
Cholesteatoma
Here, superior retraction has resulted in bony destruction in the auditory canal and an accumulation of debris in the middle ear space. Surgery is often required at this point to prevent further destruction.

Glomus Tumour
Glomus tympanicum tumours arise from the glomus bodies located in the adventitia of the dome of the jugular bulb, or along branches of the tympanic plexus. The usual presenting symptom is pulsatile tinnitus. A reddish swelling behind the tympanic membrane is often visible, and may be seen to pulsate. Early cases may be cured by surgical excision, but radiation has also been successfully employed.

Posterior Infection and Temporal Bone Fracture
In this photo, head trauma has resulted in a temporal bone fracture. Note the step deformity in the external auditory canal. The injury has also resulted in blood accumulating in the middle ear. Depending on the pathway of the fracture line, symptoms may include conductive or sensorineural hearing loss, facial paralysis, tinnitus, or vertigo. Blood in the middle ear space may be drained if it does not resolve, while conductive hearing loss may be amenable to treatment such as tympanoplasty or middle ear reconstruction. Facial nerve paralysis may require surgical intervention.
1. How is auricular hematoma most commonly managed?
Incision and drainage with pressure dressing
2. Which condition is characterized by pain and discharge, and may progress to facial nerve paralysis or other cranial nerve palsies?
Necrotizing otitis externa
3. Which condition is marked by the accumulation of blood in the subperichondrial space?
Auricular hematoma
4. If left untreated, chronic otitis media may result in…?
Retraction of the tympanic membrane
5. Which condition typically presents as a single, large pedunculated growth near the lateral end of the bony portion of the external auditory canal?
Osteoma
6. Which condition arises as the result of accumulation of hyaline material in the fibrous layer of the tympanic membrane?
Tympanosclerosis
7. The accumulation of large plugs of squamous debris and/or erosion of the bony canal is suggestive of which diagnosis?
Keratosis obturans
8. Which two conditions may present with scarring and narrowing of the external auditory canal?
Acquired stenosis and chronic otitis externa
9. What are the three potential contributing factors behind chronic otitis externa?
Recurrent acute infections, eczema, and psoriasis
10. What do we call superficial, well-circumscribed deposits in the oracle with no surrounding erythema or ulceration?
Gout tophi